Diabetes Mellitus: A Comprehensive Guide for PEBC Exam Preparation
Diabetes is a vital topic for both the PEBC Evaluating Exam (EE) and the Multiple Choice Questions (MCQ) section. Understanding its classification, management, and pharmacotherapy is critical. This guide will provide a structured approach to diabetes for exam preparation, aligned with the latest Canadian and global guidelines.
What is Diabetes Mellitus?
Diabetes mellitus is a chronic condition characterized by hyperglycemia (high blood sugar levels) due to defects in insulin secretion, insulin action, or both. Prolonged hyperglycemia can result in complications affecting the eyes, kidneys, nerves, and cardiovascular system.
Types of Diabetes
- Type 1 Diabetes Mellitus (T1DM):
- Autoimmune destruction of pancreatic beta cells, leading to absolute insulin deficiency.
- Typically presents in childhood or adolescence but can occur at any age.
- Patients require lifelong insulin therapy.
- Type 2 Diabetes Mellitus (T2DM):
- Insulin resistance and relative insulin deficiency.
- Strongly linked to obesity, physical inactivity, and genetics.
- Can often be managed initially with lifestyle interventions and oral hypoglycemic agents, but many patients progress to requiring insulin.
- Gestational Diabetes Mellitus (GDM):
- Hyperglycemia first recognized during pregnancy.
- Increases risk of developing T2DM later in life.
- Secondary Diabetes:
- Results from other conditions or medications (e.g., corticosteroids, pancreatic disease).
Diagnosis of Diabetes
The diagnosis of diabetes is based on any of the following criteria:
- Fasting Plasma Glucose (FPG) ≥ 7.0 mmol/L
- 2-hour Plasma Glucose ≥ 11.1 mmol/L during an Oral Glucose Tolerance Test (OGTT)
- A1C ≥ 6.5% (not for diagnosing type 1 diabetes)
- Random Plasma Glucose ≥ 11.1 mmol/L in a patient with symptoms of hyperglycemia
Exam Tip:
For PEBC, ensure you’re familiar with the diagnostic cut-offs for diabetes, as these are often tested in case scenarios or interpretation questions.
Non-Pharmacological Management
Non-pharmacological interventions are the foundation of diabetes management, particularly in Type 2 Diabetes. These interventions focus on controlling blood glucose levels, managing risk factors for cardiovascular disease, and preventing complications.
- Diet: Follow a balanced diet such as the Mediterranean Diet or DASH Diet that emphasizes whole grains, fruits, vegetables, lean proteins, and healthy fats. Carbohydrate counting and glycemic index are key concepts for patients with diabetes.
- Physical Activity: At least 150 minutes per week of moderate-intensity aerobic exercise, along with resistance training.
- Weight Management: Aim for 5-10% weight loss in overweight or obese patients, as this can significantly improve insulin sensitivity.
- Smoking Cessation: Reduces the risk of cardiovascular complications.
Exam Tip:
PEBC questions may ask you to recommend lifestyle interventions based on a patient’s case history. Understanding diet and exercise recommendations is key.
Pharmacological Management of Diabetes
Type 1 Diabetes
Patients with T1DM require insulin from the time of diagnosis. The insulin regimens aim to mimic physiological insulin secretion, with a combination of basal and bolus insulins.
- Basal Insulin: Long-acting insulins like glargine, detemir, or degludec provide consistent insulin coverage throughout the day.
- Bolus Insulin: Rapid-acting insulins like lispro, aspart, or glulisine are used before meals to manage postprandial blood glucose.
Type 2 Diabetes
Pharmacotherapy for T2DM typically begins when lifestyle modifications are insufficient to maintain glycemic control. Medications are selected based on patient-specific factors such as cardiovascular risk, renal function, and side effect profiles.
1. Metformin (First-Line)
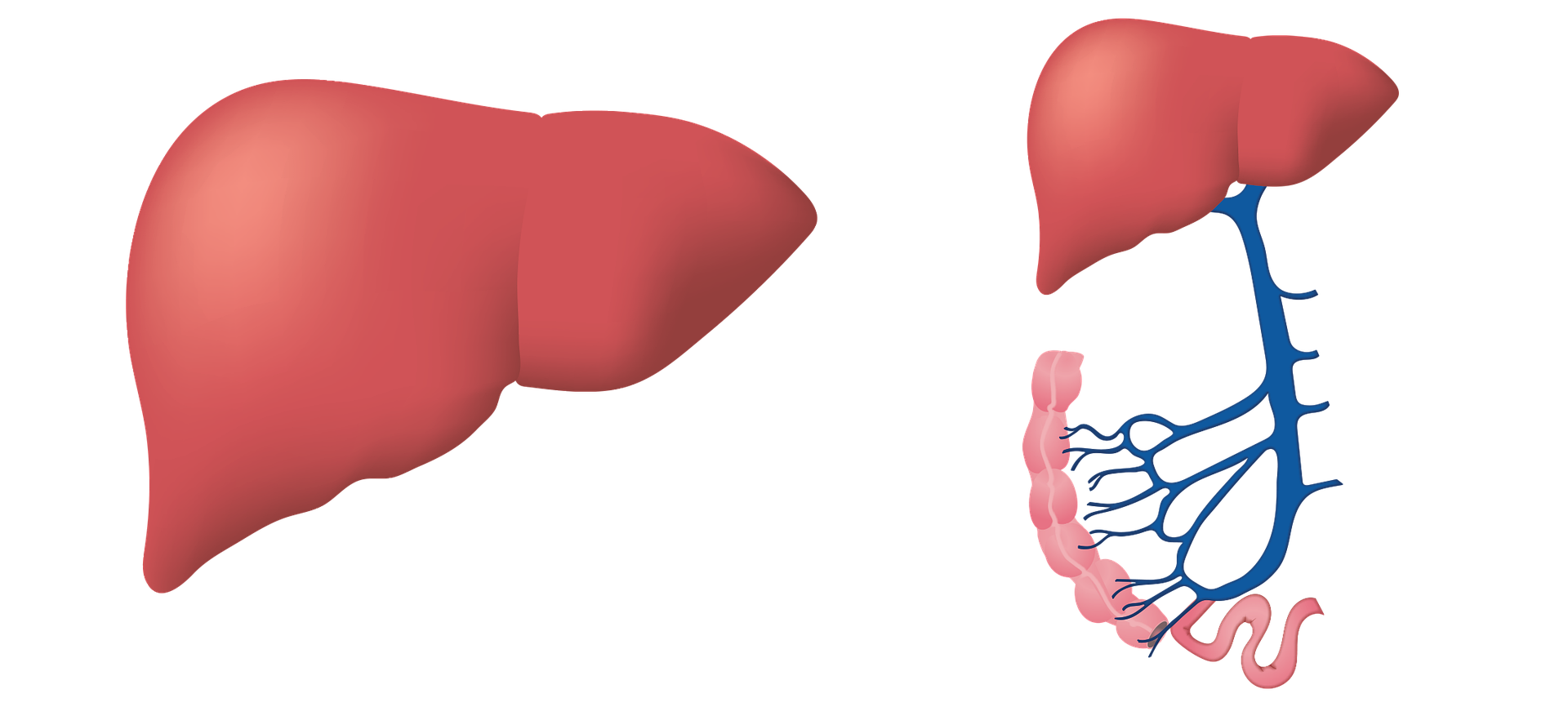
- Mechanism: Reduces hepatic glucose production and increases insulin sensitivity.
- Use: Recommended as first-line therapy unless contraindicated (e.g., eGFR < 30 mL/min).
- Side Effects: GI upset, lactic acidosis (rare).
- Monitoring: Renal function (creatinine, eGFR).
2. SGLT2 Inhibitors (e.g., Empagliflozin, Dapagliflozin, Canagliflozin)
- Mechanism: Increase urinary glucose excretion by inhibiting SGLT2 in the kidneys.
- Use: Especially beneficial in patients with heart failure or chronic kidney disease (CKD).
- Side Effects: Genital infections, dehydration, hypotension.
- Monitoring: Renal function, blood pressure.
3. GLP-1 Receptor Agonists (e.g., Liraglutide, Dulaglutide)
- Mechanism: Enhance glucose-dependent insulin secretion, delay gastric emptying, and promote satiety.
- Use: Preferred for patients with cardiovascular disease and those requiring weight loss.
- Side Effects: Nausea, vomiting, pancreatitis (rare).
- Monitoring: A1C, weight, gastrointestinal symptoms.
4. DPP-4 Inhibitors (e.g., Sitagliptin, Linagliptin)
- Mechanism: Prolong the action of incretin hormones, leading to increased insulin release and decreased glucagon secretion.
- Use: Weight-neutral option for glycemic control.
- Side Effects: Nasopharyngitis, joint pain.
- Monitoring: A1C, renal function.
5. Insulin
- May be required in patients with uncontrolled T2DM despite oral agents or in patients with significant hyperglycemia at diagnosis.
- Basal Insulin: Start with glargine, detemir, or degludec, and titrate based on fasting blood glucose levels.
- Bolus Insulin: Add prandial insulin if needed for postprandial hyperglycemia.
6. Additional Agents
- Thiazolidinediones (e.g., Pioglitazone): Enhance insulin sensitivity but can cause weight gain and fluid retention.
- Sulfonylureas (e.g., Glyburide, Gliclazide): Stimulate insulin secretion but may cause hypoglycemia and weight gain.
Combination Therapy
Most patients with T2DM will eventually require combination therapy. Common combinations include:
- Metformin + SGLT2 Inhibitor
- Metformin + GLP-1 Receptor Agonist
- Metformin + DPP-4 Inhibitor
Exam Tip:
Be familiar with the indications, mechanisms, and side effects of all major antidiabetic agents. Case-based questions in the PEBC may require you to recommend or adjust pharmacotherapy based on patient-specific factors such as comorbidities or renal function.
Monitoring and Targets
Patients with diabetes should have regular monitoring of:
- A1C: Every 3-6 months. Target <7.0% for most patients, though individualized goals may apply.
- Fasting Blood Glucose: Target 4.0-7.0 mmol/L.
- Postprandial Blood Glucose: Target 5.0-10.0 mmol/L.
- Blood Pressure: Target <130/80 mmHg in patients with diabetes.
- Cholesterol: LDL <2.0 mmol/L for cardiovascular risk reduction.
Complications of Diabetes
- Microvascular Complications:
- Retinopathy: Annual eye exams for diabetic retinopathy.
- Nephropathy: Monitor urine albumin and eGFR annually.
- Neuropathy: Regular foot exams, with patient education on foot care to prevent ulcers and infections.
- Macrovascular Complications:
- Cardiovascular Disease (CVD): Diabetes significantly increases the risk of heart disease and stroke. Consider cardiovascular protective medications like SGLT2 inhibitors or GLP-1 receptor agonists in high-risk patients.
- Diabetic Ketoacidosis (DKA):
- More common in Type 1 Diabetes, this is a life-threatening complication caused by severe insulin deficiency, leading to ketosis and acidosis.
Key Takeaways for PEBC Exams
- Know the diagnostic criteria for diabetes.
- Understand first-line and second-line pharmacotherapy and the rationale for selecting certain agents.
- Be familiar with complications of diabetes and how they are managed.
- Remember the targets for glycemic control, blood pressure, and lipid levels in diabetic patients.
By mastering these concepts, you’ll be well-prepared for diabetes-related questions in the PEBC exams!
If you haven’t sign up already, I teach people how to become a pharmacy assistant in 6 days: https://shorturl.at/VDEUQ
Get 1000 MCQ Q&A here: https://shorturl.at/ZBAQ0
Learn Antibiotics in a simplified way here: https://shorturl.at/u90BA
Top medications you should know in Canada: https://shorturl.at/3n3W0
Get a cool “Best Pharmacist In The World”: https://shorturl.at/8GgL6
Study smarter with our unique study planner” https://shorturl.at/M7hiX
References:
- Diabetes Canada Clinical Practice Guidelines: https://guidelines.diabetes.ca/
- American Diabetes Association Standards of Medical Care: https://diabetesjournals.org/care
- Pharmacotherapy: A Pathophysiologic Approach (Dipiro): https://accesspharmacy.mhmedical.com/book.aspx?bookid=1861
Disclaimer:
This blog post is intended as a study aid for students preparing for the PEBC exams and is not an official resource or endorsed by the Pharmacy Examining Board of Canada (PEBC). The information provided is based on current guidelines and best practices but should not replace official PEBC materials, textbooks, or clinical guidelines. Always refer to authoritative sources and consult professional advice for the most accurate and up-to-date information.

Very good https://is.gd/tpjNyL
Thabks Barret!