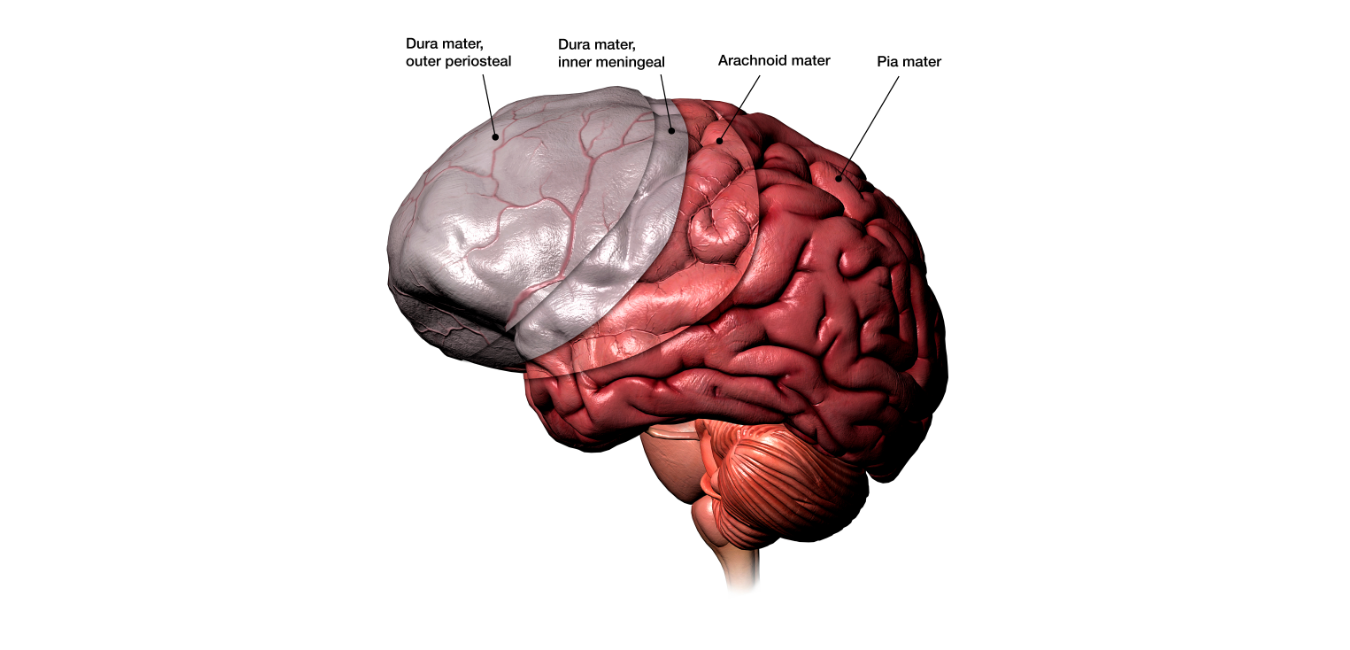
Meningitis is the inflammation of the meninges, the coverings of the brain: dura, arachnoid, and pia. It carries a high mortality rate despite medical advances.
This is a medical emergency.
Meningitis may be caused by various agents including trauma, chemicals e.g released from tumours and several infectious agents. However, bacterial meningitis represents the best known type of meningitis and perhaps, the most dangerous.
Types
– Acute
– Chronic
– Recurrent
– Post-traumatic
Terminologies
– Recurrent bacterial meningitis: new episode of bacterial meningitis occurring after a period without clinical or laboratory evidence of meningitis.
Recurrence is due to reinfection with the same or different bacterial species rather than to persistence of the original infection.
– Recrudescence denotes the reappearance, during therapy, of findings of meningitis and a positive cerebrospinal fluid culture after an initial clinical response and sterilization of the cerebrospinal fluid.
– Relapse: reappearance of bacterial meningitis within 3 weeks after completion of the initial course of therapy.
Both recrudescence and relapse are caused by the same organism isolated from the initial episode, and both represent persistence of the initial infection rather than reinfection.
Causative Organisms
The causative organisms of acute bacterial meningitis are clearly associated with the age of the patient. The common organisms in each age group are as detailed below:
Neonatal period: Escherichia coli, group B streptococci (S. agalactiae), and L. monocytogenes.
Ages 2 months to 5 years: H. influenzae
Above 5 years: S. pneumoniae and N. meningitidis.
In addition to the age of the patient, another factor that determines the causative pathogens is the presence of immunosuppression.
In immunosuppressed patients, the most frequent pathogens include L. monocytogenes (especially in patients with cell-mediated immunity deficiency), S. pneumoniae (in patients with humoral immunity deficiency), and P. aeruginosa, enteric gram-negative bacilli, and S. aureus (in neutropenic patients).
Clinical Features
The clinical features of acute bacterial meningitis vary with the age and immune status of the patient.
Children may present with fever, convulsions, refusal of feeds, irritability, excessive cry and vomiting.
Adults may present with fever, headache, vomiting, lethargy, confusion, and a stiff neck.
The manifestations, however, may be subtle, especially in newborns, immunosuppressed patients, and the aged.
In addition, patients who develop meningitis after head trauma or neurosurgical procedure may have features that are difficult to distinguish from the underlying pathology. As such, a high index of suspicion is needed in this category of patients to make a early diagnosis.
Clinical examination may reveal neck stiffness/retraction, positive Kernig’s and Brudzinski signs and features of acute ill-health with deranged neuro-vital signs.
Diagnosis
The definite diagnosis of bacterial meningitis is based on the findings of cerebrovascular fluid (CSF) examination. The CSF is obtained from lumbar puncture.
The usual picture is pleocytosis with cell count over 1,000 cells per mm3 (with polymorphonuclear cells predominating), hypoglycorrhagia with glucose under 30 mg per dL and elevated protein usually over 200 mg per dL. Gram staining and microscopy may reveal the causative organism.
Differential Diagnosis
– Systemic Lupus Erythematosus and other connective tissue diseases
– Drug-induced meningitis
– Tumours
– Epidermoid & Parasitic cysts
Treatment
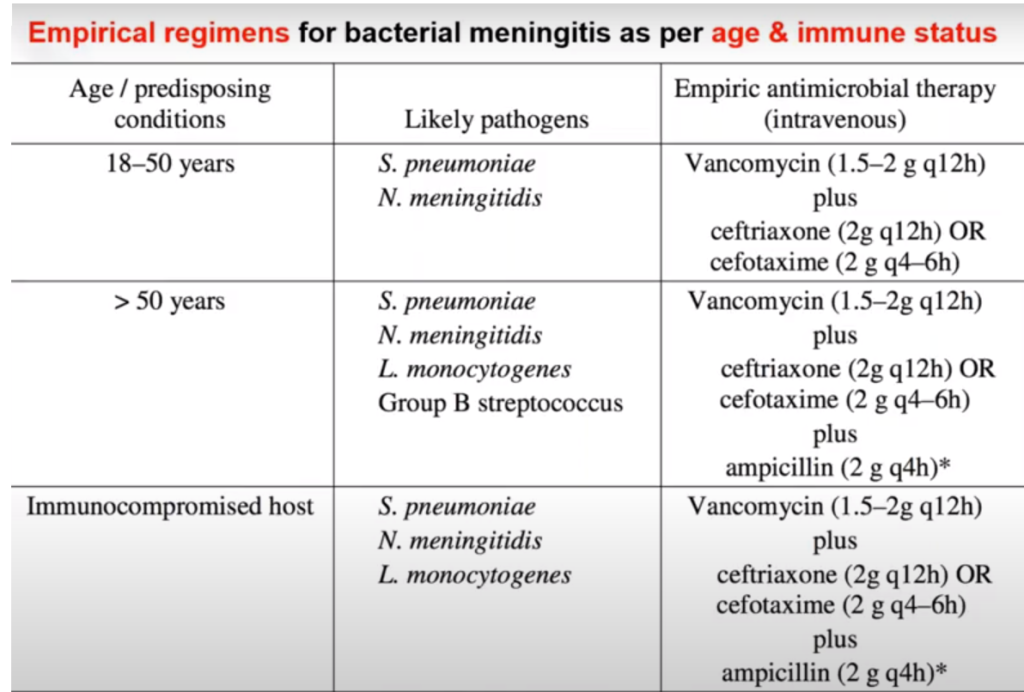
Antibiotics are the mainstay of treatment of bacterial meningitis. It is essential to use antibiotics which readily cross the blood brain barrier. The third generation cephalosporins are in wide use for the treatment of meningitis especially in adults.
Broad-spectrum agents are used initially, while specific drugs are commenced as soon as results of CSF analysis are available.
The use of corticosteroids in the management of bacterial meningitis is controversial. While some studies have documented its benefits, especially reduction in hearing impairment, others have not found it so useful. If dexamethazone is to be used, it needs to be started before, or along with the first dose of antibiotics to reduce the patient’s inflammatory response.
DISCLAIMER
All content and information on this website are for informational and educational purposes only.
It does not constitute medical, psychological, or health advice of any kind and we do not warrant that the information presented herein is free of any errors or omissions.
We are not providing medical, health care, nutrition therapy, or coaching services to diagnose, treat, prevent or cure any kind of physical ailment, mental or medical condition.
Although we strive to provide accurate general information, the information presented here is not a substitute for any kind of professional advice, and you should not rely solely on this information.
Always consult a professional in the medical and health area for your particular needs and circumstances prior to making any medical or health-related decisions.
What to read next?
https://simplifiedpharmacy.com/blog/
